Research at a glance and key statistics
How to lose weight after a hysterectomy is a common concern—many struggle with post-hysterectomy weight gain or worry it’s unavoidable. The good news: steady, science-based habits can help you maintain or lose weight without extreme diets or giving up everything you love.
Disclosure: This article contains affiliate links. We may earn a commission at no extra cost to you.
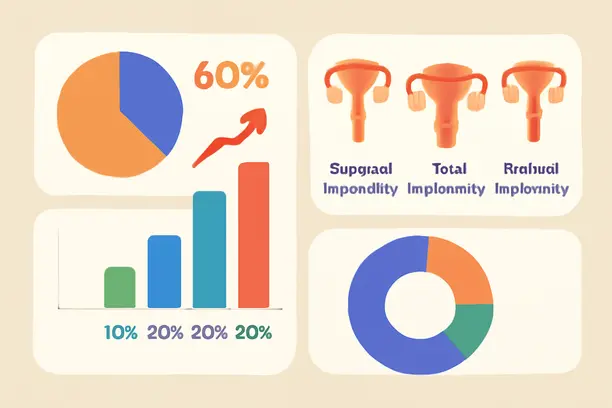
Weight gain after hysterectomy varies widely. Most women gain only 2 to 5 pounds within the first year. However, about 20% to 25% may see a bigger shift—10 pounds or more. These findings come primarily from mid-2000s studies, so they reflect a nuanced picture: weight gain isn’t inevitable or dramatic for everyone, but your individual risk factors and lifestyle choices matter deeply.
Several things influence the likelihood and amount of weight change, including the type of hysterectomy you have, your baseline health, and how active you stay. Surgical advances and improved post-operative care may further reduce these risks. Understanding your personal profile empowers you to take targeted, sustainable steps.
Key Statistics at a Glance
- Most women gain 2–5 pounds within 12 months; nearly 1 in 4 may gain 10 or more.
- Total hysterectomies tend to carry a higher risk than partial or laparoscopic procedures, though less invasive methods may narrow this gap.
- Some individuals actually lose weight following surgery, often due to improved health or lifestyle changes.
- Older studies reflect less diverse populations and surgical techniques, so results may not fully represent modern outcomes.
Understanding these general trends alongside your unique situation helps you craft a thoughtful post-operative plan.
For practical support, exploring meal plans that emphasize satiety and balanced nutrition can be beneficial. For example, family-friendly healthy meals can help you maintain stable eating routines after surgery.
Context and Limitations of Current Knowledge
Most existing research predates widespread adoption of minimally invasive techniques and enhanced recovery protocols. These advances likely influence weight outcomes, but comprehensive long-term data is still awaited.
Prevention and reversal of weight gain after hysterectomy remain achievable. Structured, satiety-focused dietary programs like the 14-Day Rapid Soup Diet can provide accessible starting points to support gentle, effective weight control post-surgery.
Recognizing the evidence-backed odds and your individual context gives you a strong foundation for realistic, sustainable weight management after hysterectomy.
Hysterectomy types, ovarian status, and how hormones affect weight
The specific nature of your hysterectomy profoundly affects your hormone balance, metabolism, and consequent weight changes. Whether your ovaries remain or are removed shifts how estrogen and other hormones regulate your appetite, fat distribution, and energy use.

- Uterus removed, ovaries retained: Estrogen production continues, so hormonal disruption is less pronounced. Weight gain risk is generally lower but still influenced by age and natural menopause timing.
- One ovary removed: Hormone levels may fluctuate mildly, but surgical menopause is generally avoided.
- Both ovaries removed (bilateral oophorectomy): Immediate surgical menopause results in steep drops in estrogen and progesterone, often triggering rapid metabolic shifts, muscle loss, fat redistribution toward the abdomen, hot flashes, and mood changes.
The surgical approach also matters. Abdominal hysterectomies usually require longer recovery with restricted activity, which limits early exercise. Vaginal and minimally invasive methods often enable a quicker return to movement, aiding weight management.
How Estrogen Shifts Affect Body Composition
Estrogen plays a central role in directing how and where your body stores fat. Its sudden loss—common after bilateral oophorectomy—often promotes abdominal fat accumulation, a pattern linked to increased cardiovascular and metabolic risks.
- Fat redistributes to belly and waist areas.
- Basal metabolic rate declines, reducing calories burned at rest.
- Lean muscle mass decreases without strength training.
- Symptoms like hot flashes, sleep disruption, and mood fluctuations may impact appetite and energy.
Hormone replacement therapy (HRT) may help mitigate some metabolic and symptomatic changes, but it requires careful, personalized discussion due to varying risks and benefits.
Practical Post-Surgery Expectations
- Recovery time: Typically 2–8 weeks; abdominal surgeries require longer rest than minimally invasive ones.
- Activity: Walking often starts earlier with less invasive methods; heavy lifting and strenuous exercise should wait until clearance.
- Symptoms: Surgical menopause can cause rapid weight and mood changes—early recognition aids management.
- Hormone therapy: Consultation recommended if both ovaries are removed, especially for women under 50.
- Monitoring: Track waist size, muscle loss, cravings, and energy to guide lifestyle adjustments.
Tailored meal plans like the 14-Day Rapid Soup Diet can complement recovery and dietary needs during this transitional phase. Additionally, Mediterranean diet principles support hormonal balance and anti-inflammatory benefits.
If you’re looking for a gentle, structured way to regain control over cravings and energy, try a soup-based meal plan designed for busy recovery days. It’s a low-impact way to feel full and supported, even when your energy fluctuates.
Who’s at higher risk — baseline health, life stage, and equity considerations
Not all women face the same challenges managing weight after hysterectomy. Your pre-surgery health, hormonal status, and social factors all influence risk and outcomes.
Higher risk groups include women with pre-existing obesity, insulin resistance (e.g., PCOS, diabetes), or a history of weight cycling. Hormonal transitions around menopause also exacerbate metabolic slowdowns and abdominal fat gain. These factors make individualized planning essential.
- Metabolic conditions: Blood sugar issues require medical and nutritional review for tailored insulin stabilization strategies.
- Perimenopausal or menopausal stage: Discuss hormone balancing and nutrition with healthcare providers; maintaining consistent, gentle activity remains key.
- History of yo-yo dieting: Behavioral therapy or team-based care may assist with sustainable habit formation.
- Lifestyle risks: Smoking, sedentary habits, and older age benefit from early micro-habits like brief walks and smoking cessation support.
Health equity issues also affect outcomes. Black women and those from lower socioeconomic backgrounds often experience higher hysterectomy rates but face limited access to tailored post-operative care and resources. Educational gaps, insurance barriers, and fewer local weight management programs may create additional challenges.
Community support, advocacy organizations, and trusted online plans such as the Rapid Soup Detox can help bridge resource gaps and provide practical, time-efficient guidance for diverse populations.
Ultimately, post-hysterectomy weight risk arises from a blend of biology, life stage, and social context. Self-advocacy, connection to specialized care, and culturally sensitive support are crucial components of success.
Need a starting point that doesn’t require hours of meal prep or expensive groceries? Explore a simple soup plan that’s easy to follow and budget-friendly—it’s designed for real-life challenges and busy schedules.
Post-op recovery stages and a pelvic‑floor‑aware exercise progression
Recovery from hysterectomy proceeds through defined phases and requires patience and attentiveness to your body. Tailoring activity to your surgery type—abdominal, laparoscopic, or vaginal—supports safe healing and eventual weight management.
- Weeks 0–2: Gentle Movement
Engage in slow walking, standing breaks, ankle pumps, and gentle stretches without straining abdominal or pelvic muscles. Protecting the surgical wound and pelvic floor is paramount. Watch for fever, bleeding, or unusual pain; contact your care team if these arise. - Weeks 3–6: Core and Pelvic Floor Engagement
Begin gentle pelvic tilts, abdominal bracing, and pelvic floor activation (e.g., connection breathing or Kegels) if comfortable and approved. Light household tasks and short walks may be appropriate. Avoid resistance or impact exercises. - Weeks 6–12+: Gradual Strength Building
With surgeon approval, introduce bodyweight exercises, light weights, or resistance bands while guarding pelvic floor safety. High-impact or heavy lifting remains contraindicated until cleared. Longer recovery may be needed for abdominal surgery cases or complications.
Protecting the Pelvic Floor
Removal of the uterus changes pelvic floor dynamics, increasing risk for strain or prolapse, particularly during exercise. Symptoms such as pelvic pressure, bulging, or urinary leakage signal a need to pause and seek pelvic floor physical therapy. Specialists can guide safe progressions and optimize recovery.
At-home gentle core exercises designed for safety help rebuild strength while minimizing pelvic stress.
Check This
- 7 Minute Workout for Women: Sculpt, Tone and Burn Fat in Record Time
- Top 10 Gluten Free Lean Cuisine Meals for Easy, Healthy Weeknight Dinners
Exercise and Weight Loss Considerations
Post-surgery metabolic rate often temporarily decreases due to muscle loss and reduced movement. Aggressive dieting or rapid high-intensity workouts can be counterproductive. Focus first on walking, portion control, and nutrient-dense meals.
Over time, incorporate strength training combined with pelvic floor coordination to rebuild muscle and revitalize metabolism for enduring weight loss success.
When to Seek Extra Guidance
Contact your clinician if you experience fever, severe pain, shortness of breath, bloating, persistent pelvic floor symptoms like leaking or heaviness, or if recovery stalls. Prompt specialized physical therapy referrals and medical support can prevent complications and support smoother progress.
Structured, easy-to-follow programs—such as the 14-Day Rapid Soup Diet—offer practical meal plans that align with recovery needs and support steady weight loss.
Nutrition, medications, supplements, and realistic weight‑loss expectations
Setting practical, safe weight-loss expectations after hysterectomy is essential. Most experts recommend gradual loss of 0.5 to 1 pound per week once you’re cleared for active management. Rapid weight loss is rarely advised, as hormone shifts and metabolic changes affect your body’s responsiveness and healing.
Nutrition First: Foundational Strategies
A balanced diet emphasizing whole foods—lean protein, fiber-rich vegetables, whole grains, and healthy fats—supports recovery and sustainable weight loss. Limiting processed foods and sugary drinks helps manage calorie intake.
Structured, satiety-focused meal plans such as those relying on nutrient-dense soups can facilitate portion control and appetite management during recovery.
Supplements: Use with Caution
Although supplements promise benefits, many lack proven efficacy or safety. Some, like high-dose green tea extract or diuretics, may adversely affect heart or liver function. Calcium and vitamin D support bone health but should be supplemented only if indicated by blood tests or dietary gaps.
Always discuss supplements with your healthcare provider, especially those advertised for metabolism or hormonal balance, as interactions and contraindications exist. The FDA doesn’t regulate most weight-loss supplements for safety or efficacy, so choose brands with third-party verification.
Medications for Weight Loss
If lifestyle changes alone aren’t sufficient and you have BMI ≥30 (or ≥27 with related health conditions), FDA-approved medications such as orlistat, phentermine/topiramate, naltrexone/bupropion, or GLP-1 agonists (e.g., semaglutide) may be options. These reduce appetite or slow digestion but carry side effects like nausea or rare thyroid concerns.
Medication requires careful screening and ongoing physician oversight. Not everyone qualifies, especially those with certain heart conditions or substance histories. Avoid initiating treatments without thorough, shared decision-making.
Hormone Therapy and Surgery for Weight Loss
Hormone replacement therapy (HRT) can alleviate menopausal symptoms post-hysterectomy but isn’t intended for weight loss. It carries risks—including blood clots and certain cancers—and should be used only after medical consultation.
Bariatric surgery is a last resort, reserved for severe obesity and related illnesses after other methods are exhausted. Hysterectomy-induced weight gain alone isn’t indication for surgical intervention.
Safe Diet Plans and Detoxes
Long-term weight control depends on individualized, sustainable nutrition and behavior changes. Short-term structured diets, like the 14-Day Rapid Soup Diet, can offer convenient support for appetite control without harsh restrictions.
Avoid crash diets or miracle supplements; prioritizing nutrient density, portion control, and consistent habits leads to the best outcomes.
Let’s keep this doable: small, steady changes and the right plan can help you feel in control again.
Emotional health, body image, and when to contact your clinician
Weight and body changes after hysterectomy often affect emotional well-being and self-image. Feelings of disconnection, frustration, or mood swings are common responses to surgical and hormonal transitions. You’re not alone in this.
Accepting that recovery includes psychological shifts reduces internal pressure and supports resilience during setbacks.
- Cognitive tools: Practice reframing negative thoughts, such as “My value isn’t defined by weight,” and cultivate gratitude focused on bodily function and health.
- Support networks: Engage with peer groups sharing similar experiences for encouragement and practical advice.
- Gentle goal setting: Celebrate non-scale victories like improved energy or mood.
If persistent low mood, anxiety, or emotional eating lasts beyond two weeks, seek counseling or healthcare support. Therapy equips you with coping strategies that protect healthy eating and activity routines.
When to Contact Your Clinician
Contact medical professionals promptly for:
- Rapid weight gain of 5–10 pounds with swelling, leg puffiness, or shortness of breath—possible signs of fluid retention requiring urgent evaluation.
- Ongoing nausea, inability to eat, or nutritional failure.
- Persistent weakness, dizziness, or fatigue that rest doesn’t improve.
- Infection signs at the incision, such as redness, swelling, discharge, or foul odor.
- Severe emotional distress, suicidal thoughts, or inability to cope—call emergency or mental health services immediately.
Maintain a daily log of weight, swelling, mood, wound status, and appetite to aid your clinician’s assessment and personalize care.
Building Daily Habits for Long-Term Success
Small, consistent self-care steps support mood and motivation. Structured plans like the 14-Day Rapid Soup Diet provide comforting meal ideas and reduce food-related stress during recovery.
Seeking mental health assistance is a sign of strength. Tools to boost workout motivation and maintain consistency are valuable resources as you regain balance post-surgery.
Remember: recovery encompasses your whole self—physical, emotional, and mental health. Collaborating with your healthcare team ensures a supportive, individualized path forward.
If you want a meal plan that fits real life—no equipment, no gym, just gentle structure—consider starting with a 14-day soup protocol for comfort and control. It’s joint-friendly and lets you pick up where you left off, even if you miss a day.
Ready to take control? Start your gentle weight-loss reset today
You’ve learned what influences post-hysterectomy weight gain—and that managing it doesn’t require drastic measures or endless frustration. A structured soup plan can help you regain control, boost energy, and support steady weight loss without the overwhelm or harsh restrictions.
Try it risk-free: get instant access to the full 14-Day Rapid Soup Diet, including recipes and follow-along videos. There’s a 60-day money-back guarantee, so you can see if it fits your needs without pressure.

